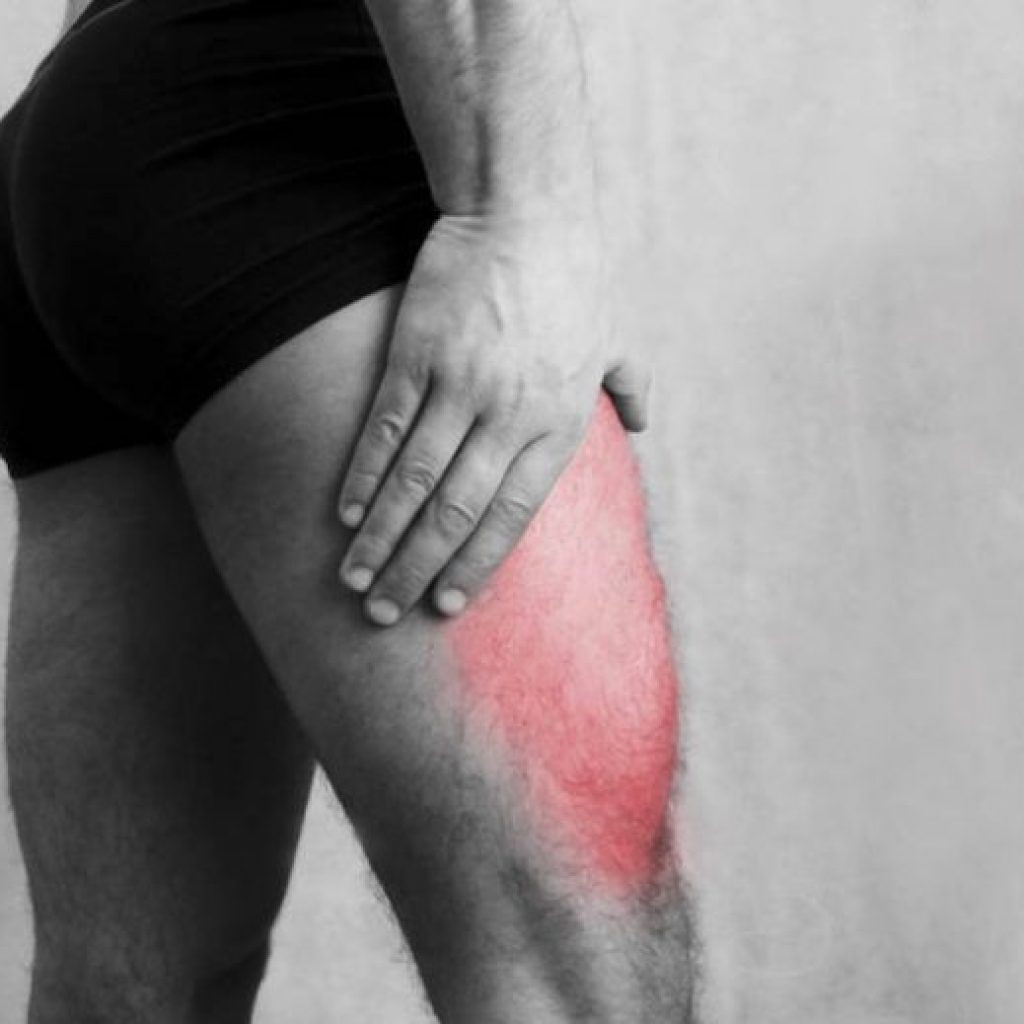
Meralgia paresthetica is defined as a compression or entrapment of the femoral cutaneous nerve that causes paraesthesia (“numbness”), tingling, loss of sensation, and sometimes pain in the anterolateral aspect of the thigh. Approximately 20% of the cases occur bilaterally in both lower limbs.
A specific origin of this pathology is not known, but scientific evidence subdivides two possible causes:
- Spontaneous: Any factor that can increase intra-abdominal pressure at the level of the pelvis can cause compression of the femoral nerve branch due to space reduction.
It can originate from:
- Increased pressure due to internal causes: obesity, pregnancy, mass…
- Increased pressure due to external causes for e.g., use of very tight clothing that causes pelvic compression (pants, belts, corsets, military/police uniforms…).
- Bone abnormalities that can decrease space and increase pressure.
- Iatrogenic: Bone surgeries of the pelvis or spine.
In turn, metabolic disorders such as diabetes or the consumption of alcohol and tobacco can increase the predisposition to suffer from this pathology.
At Archview Physiotherapy, we provide treatments, such as:
Manual treatment of soft tissues and fascial system: It is necessary to work on the muscle tissue that may be compressing the affected femoral nerve branch.
Mobilization: We will work the mobility of the hip and pelvis
Dry needling applied to trigger points of the muscles that are directly related to pain in that area.
Neurodynamic. Which helps to reduce symptoms (paraesthesia or pain) and improving mobility.
Exercise: to improve lumbopelvic stability and the function of our legs.
To book an appointment with one of our team at Archview Physiotherapy Pain and Sports Injury Clinic, please call 014913228 or book online www.archviewclinic.ie. Located in Ranelagh, Dublin 6.