Written by Amanda Olsen
Did you know that your pelvis can go out of alignment? It occurs more often than you’d think, and can be a cause of certain ailments/pain OR can be the result of other issues occurring in your body.
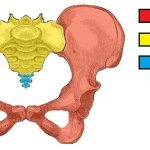
A general overview of the anatomy of the pelvis…
– The pelvis, or “the pelvic girdle” is made up of three components: the two hip bones (the ilia), the sacrum, and the coccyx (your tail bone).
– The area where the sacrum meets the hip bone (ilia) is called the sacroiliac joint (dimples at low back).
o This is the most common place for dysfunction to occur in the pelvis – this joint can also refer pain into the low back
– These three components are held together by many ligaments and muscles
What happens?
– Whether due to a sudden traumatic experience (i.e. car crash, landing forcefully on one leg) or a prolonged onset from muscle imbalances, the pelvis can become mal-aligned
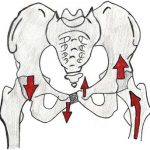
– The different types of mal-alignment are:
o Upslip: one hip is higher than the other
o Forward/backward rotation: one side of pelvis is either more forwards or more backwards than the other side
o Inflare/Outflare: one side of pelvis either flares out from mid-line more or more towards mid-line more than the other side
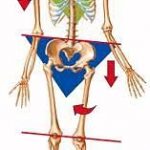
o Leg Length Discrepancy: one leg may be longer than the other because of a forward rotation of the pelvis on the side of the longer leg
o Sacral torsion: the sacrum is tilted or rotated more to one side
Signs & Symptoms:
– Pain at site of sacroiliac joint (dimples of low back)
– Low back pain
– Buttock pain
– Feeling “off kilter” or “out of balance”
How physiotherapy can help:
– Your physiotherapist will carry out several tests and measures to determine if you have a pelvic mal-alignment that could be causing your current symptoms
– If a mal-alignment is confirmed, the following things can be done for it:
o Muscle Energy Techniques: there are a few, but the one specific to your findings is the one that will be used – this helps get the pelvis back into alignment
o Dry Needling: if muscle tightness is causing the mal-alignment then dry needling will help loosen it out and its hold on the pelvis will be released
o Trigger point/myofascial release: alternative to dry needling where the therapist’s hands are loosening out the muscle and connective tissue around it
o Exercises: specific exercises will be given to you based on what the findings are, and are tailored to keep the pelvis in its corrected alignment
Having a pelvic mal-alignment can create a knock-on effect to the back, hips, knees, and feet. So if you are experiencing any of these, it’s possible that your pelvis needs to be corrected!